By NAHEEM NOAH
A Name from the Black Gap
Three months into constructing Carenector’s facility-to-facility platform, I obtained a name that crystallized the whole lot fallacious with healthcare referrals. A hospital social employee, who was already utilizing our particular person affected person platform to assist households discover care, had been making an attempt to coordinate an institutional placement for an 82-year-old stroke affected person for six days. She’d made 23 cellphone calls. Despatched 14 faxes. The affected person was medically cleared however caught in an acute mattress costing $2,000 per day as a result of nobody may verify which expert nursing amenities had open beds, accepted her Medicaid plan, and had stroke rehabilitation capability.
“I really like what you constructed for sufferers,” she informed me, “however once I have to do a facility-to-facility switch, I’m again to faxing. Can’t you repair this workflow, too?”
She wasn’t fallacious. We’re in 2025, and regardless of billions poured into well being IT and breathless AI guarantees, referring a affected person usually seems like stepping again into 1995. Earlier this yr, THCB’s personal editor Matthew Holt documented his try and navigate specialist referrals by means of Blue Defend of California. The echocardiogram referral his physician despatched by no means arrived on the imaging heart. When he wanted a dermatologist, his medical group referred him to a supplier who turned out to not be lined by his HMO plan in any respect. “There’s a large alternative right here,” Holt concluded after his odyssey by means of disconnected methods, “though we’ve obtained now numerous the info…to combine it and make it helpful for sufferers.”
Clinicians make over 100 million specialty referrals yearly within the U.S., but analysis exhibits that as many as half are by no means accomplished.
Right here’s what we’ve realized after a yr of operation: we constructed a consumer-facing platform that helps people and households discover care suppliers matching their wants, insurance coverage, and placement—it now serves over 100 each day customers, together with sufferers, social employees, and discharge planners. However fixing particular person care searches is just half the battle. The institutional referral workflow—hospital to expert nursing facility, SNF to rehab heart, clinic to specialist—stays trapped in fax machines and cellphone tag as a result of nobody redesigned the precise coordination course of.
That’s what we’re constructing now. And the query haunting us isn’t why we don’t have higher instruments? It’s why billions in AI funding left the institutional referral workflow nearly unchanged?
The Structure of Failure
The reply isn’t about smarter algorithms or shinier dashboards. It’s a few elementary mismatch between how AI will get deployed and the way care coordination really works.
Begin with the info layer. One survey discovered that 69% of major care physicians say they “at all times or more often than not” ship full referral notes to specialists, however solely 34% of specialists report receiving them. Even inside a single hospital system, info routinely vanishes at handoff factors. Matthew Holt skilled this firsthand when his physician’s referral for an echocardiogram merely by no means arrived on the imaging heart, regardless of prior authorization from Blue Defend already being within the system.
However the fragmentation goes deeper than lacking referrals. When Holt’s medical group referred him to a dermatologist, they despatched him to a supplier not lined by his HMO plan, though the EMR had his insurance coverage info and member ID. As he documented“there’s a large alternative right here…most of this information about who I ought to go and see…is all obtainable. It’s simply not made very apparent in anyone place.” Medical teams, hospitals, and well being plans every keep their very own methods, with no real-time integration to reply the easy query: Is that this supplier in-network for this affected person’s plan?
Then there’s the inducement drawback. A 2022 analysis of CMS’s Complete Major Care Plus initiative discovered zero affect on care fragmentation. The researchers concluded that “excessive ranges of fragmented care persist” as a result of cost fashions don’t sufficiently reward suppliers for really closing referral loops. No person will get paid to chase down a misplaced referral, so referrals slip by means of the cracks.
Lastly, there’s the cussed analog actuality: over half of referral handoffs nonetheless occur by fax (56%) or paper handed to sufferers (45%). We haven’t rewired the workflow; we’ve simply digitized the mess.
Why “AI-Powered” Options Preserve Failing
Given these issues, you’d anticipate AI distributors to swoop in with options. As an alternative, most have made issues worse by treating AI as an add-on quite than infrastructure.
The standard strategy: OCR to scan paper referrals, auto-fill widgets for EHR fields, predictive algorithms for threat scoring. Every device solves a micro-problem whereas ignoring the macro-disaster. As one Innovaccer evaluation put ithealthcare AI dangers “repeating previous errors, with disconnected instruments creating inefficiencies as an alternative of options.”
McKinsey’s latest evaluation makes the identical level: the widespread adoption of AI-enabled level options “is creating a brand new fragmentation drawback.” The trail ahead isn’t extra remoted instruments however “assembling these capabilities right into a modular, related AI structure.” And with out information interoperability, none of this issues. As Innovaccer bluntly states“With out clear information, true interoperability is fantasy. With out interoperability, AI is simply costly noise.”
What We’re Constructing—Knowledgeable by 100+ Day by day Customers
Our client platform taught us one thing essential: whenever you give individuals (and the social employees serving to them) a device that really matches their must obtainable suppliers in real-time, they use it. Day by day. Over 100 customers now depend on Carenector to navigate post-acute care, rehabilitation providers, and specialist referrals primarily based on their insurance coverage, location, and medical necessities.
However those self same social employees saved telling us, “This works nice once I’m serving to a member of the family search on their very own. However once I have to coordinate a hospital discharge or facility switch on behalf of my group, I’m again within the Stone Age.”
That’s why we’re now constructing the facility-facing platform, and we’re doing it in another way than our first try. We’re not guessing at what hospitals want. We’re testing actively with a choose group of companion amenities, incorporating steady suggestions from their case managers and discharge planners who’ve seen what works within the client product.
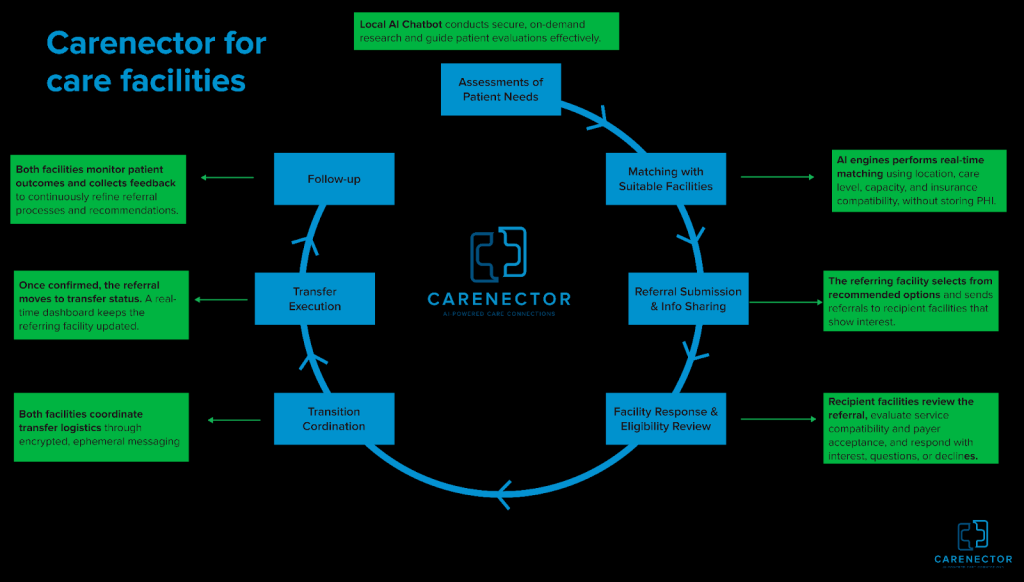
The Facility Workflow We’re Constructing
As an alternative of bolting AI onto current chaos, we’re rebuilding the institutional referral course of end-to-end. Care groups enter structured affected person wants—diagnoses, rehab necessities, gear, insurance coverage sort, location—with out sharing any personally identifiable info. No names, no medical report numbers, no birthdates within the preliminary matching section. Our AI engine performs real-time constraint-aware matching primarily based purely on scientific and logistical standards: if a affected person wants expert nursing with PT providers, accepts solely particular Medicare plans, requires Spanish-speaking workers, and have to be inside 10 miles, the system surfaces solely amenities assembly each criterion concurrently.
As soon as matches are discovered, referring amenities ship inquiries by means of safe channels with either side seeing the identical standing timeline. We’ve constructed ephemeral messaging threads the place nurses and consumption coordinators talk in real-time, no extra fax-into-void questioning. After a facility accepts, the whole lot stays in a single thread: transport scheduling, medicine reconciliation, and insurance coverage verification.
Right here’s what makes this clever: we monitor whether or not placements succeed or fail. Did the affected person get readmitted inside 30 days? Did the power’s providers match what was promised? That end result information feeds again into the matching algorithm, progressively studying which amenities ship on their commitments.
What We’re Studying in Actual-Time:
We’re constructing and testing the power platform with a choose group of companion hospitals and expert nursing amenities. This isn’t broadly obtainable but. We’re iterating quickly primarily based on steady suggestions from these early adopters, and the teachings are reshaping our strategy:
- Belief requires transparency. Our early facility matching AI was a black field—”belief us, these are good matches.” Adoption amongst our pilot companions was horrible. Once we added transparency exhibiting why every facility matched primarily based on which particular standards, engagement jumped. Case managers need to see the system’s reasoning, not simply its suggestions.
- Privateness is about good defaults, not paranoia. We initially constructed maximalist privateness controls that made the workflow clunky. Steady suggestions from our testing companions taught us the correct strategy: begin with zero PII within the matching section, amenities see solely scientific and logistical standards. Share affected person identifiers solely after a facility signifies curiosity and capability, utilizing expiring entry and audit logs. This center path eliminates the referral black gap (amenities can reply rapidly with out regulatory considerations) whereas defending affected person privateness the place it issues most.
- The true barrier isn’t know-how—it’s adoption technique. One social employee in our pilot saved faxing alongside our beta platform. Three weeks into testing, after seeing 4 profitable placements coordinated by means of our system, she stopped faxing. The tech didn’t change. Her confidence did. We’re studying to measure success not in options shipped however in workflows deserted.
Past Expertise: What the System Wants
Even the best-designed AI received’t repair referrals alone. The ecosystem wants parallel adjustments:
- Regulatory reform: CMS may require digital referral monitoring as a situation of participation and pay suppliers for profitable referral completion, not only for encounters.
- Requirements adoption: FHIR APIs and HL7 interoperability requirements exist however stay non-obligatory. Necessary adoption would let completely different distributors’ methods really discuss to one another.
- Shared accountability: The most important cultural shift wanted is shifting from “I despatched the referral” to “I confirmed the affected person obtained care.” ACOs and value-based contracts are nudging this course, however slowly.
From Band-Aids to Rebuilt Plumbing
That 82-year-old stroke affected person? She obtained positioned on day seven by means of the social employee’s fax machine. The delay value the hospital $14,000 in extra acute care days. Multiply that throughout tens of millions of referrals yearly and also you glimpse the financial waste embedded in our infrastructure.
The know-how to repair this exists—real-time information pipelines, constraint satisfaction algorithms, safe messaging, end result analytics. What we haven’t had is the need to reassemble these items into coherent workflows as an alternative of piling them onto damaged processes.
Our client platform proved that whenever you rebuild the search and matching layer from scratch, individuals undertake it. Now we’re testing whether or not the identical strategy works for institutional coordination with a choose group of pilot amenities. The early alerts from these companions are promising, case managers who use each our merchandise inform us the power platform seems like a pure extension of what they already belief.
The toughest conversations aren’t with engineers, they’re with hospital directors who’ve been burned by “AI options” that promised transformation and delivered costly shelfware. We don’t lead with AI anymore. We lead with a query: When your case supervisor sends a referral, do they know—with certainty—that it was acquired, reviewed, and acted on? For many hospitals, the reply isn’t any. That’s the issue we’re fixing with our pilot companions.
If we succeed, it received’t be as a result of we constructed a better algorithm. It’ll be as a result of we rebuilt the plumbing primarily based on what actual customers informed us they wanted. And if we fail? It’ll most likely be as a result of we forgot that know-how isn’t the toughest a part of healthcare—belief is.
Naheem Noah is a PhD researcher on the College of Denver and co-founder of Carenectora healthcare referral platform.

